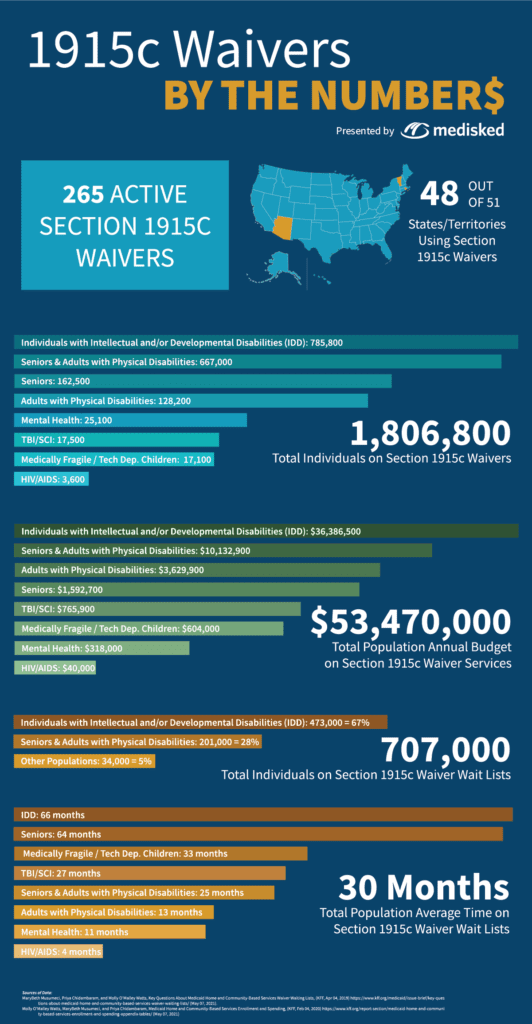
Across the United States, there are over 800,000 individuals waiting for waiver services and the number grows each year. These are individuals who have indicated they have a need for services to keep them safely in their homes but are waiting for communication from their state Medicaid agency that funding has been made available. Some individuals are waiting up to five years or more for funding.
The Biden administration has been taking big steps in their first few months in office to build up the availability, sustainability, and infrastructure surrounding home and community-based services (HCBS). The American Rescue Plan includes $400 billion of extra funding to support HCBS—that’s billion with a “b.” While home and community-based services have gained popularity over the last few decades, it has taken quite some time to make real progress. This additional funding could make a huge difference in access to services.
This extra funding has the potential to make an impact from several angles:
- Currently, the extension of the Money Follows the Person program is set to expire in 2023. This program, intended to support individuals being deinstitutionalized, has gone through a series of short-term extensions, making it difficult for states to continue the momentum with the program. The funding could make a successful program within Medicaid permanent.
- The direct support professional (DSP) workforce crisis, in which there are not enough willing and qualified providers available to support the number of individuals requiring services, has been an ongoing issue for the HCBS world. The funding will likely be allocated to provide better wages to workers, sick pay, and training which will go a long way in the retention and professionalization of this career path.
- Medicaid programs will be able to expand the availability of services in both number and type. States may finally be able to address their wait lists and bring individuals onto the waiver which not only supports them in their home but reduces the risk of institutionalization as well.
States have broad flexibility in developing their waiver programs. The number of waivers they implement, target populations, the definitions, and required criteria for eligibility make comparing wait lists across states an apples to oranges situation. While most states have waivers for the IDD, older adult, and physical disability populations, other target groups are not as prevalent or consistent across states. Using a technology platform that is flexible enough to apply eligibility criteria across waiver programs makes it easy to manage all waivers and view reports about the number of individuals on each wait list, their location within the state, and the average wait time for a slot.
The State Medicaid Agency or other operating agencies which administer waivers are typically operationally siloed and often use different technology platforms. This may lead to a larger number of individuals on wait lists since individuals may be on more than one list. The ability to manage oversight of all wait lists for all waivers a State Medicaid Agency is responsible for, allows for better and more accurate reporting which can influence future amendments including increases in the number of slots for a particular waiver. These wait lists can be streamlined when State agencies utilize technology that manages all wait lists within one platform.
Processes play a part when it comes to more accurately and clearly identifying individuals to place on wait lists. Currently, 31 states screen individuals for waiver eligibility prior to placement on a wait lists, while nine states do not. The nine states that do not screen for waiver eligibility make up 57% of the total waiting list population.[1] States that do screen for waiver eligibility can quickly communicate eligibility to the individual when a slot becomes available. In addition, screening can enable agencies to assist individuals with linkages to other services if they are not waiver eligible.
As additional funding becomes available to states, they will need to be prepared to manage existing wait lists as well as an influx of newly eligible individuals if eligibility is expanded. MediSked is poised and positioned to support states through this evolution. MediSked offers waiver management functionality that can support multiple waivers at a time and can be configured to reflect the unique rules for entry onto a waiver in any particular state.
[1] Musumenci, M., Chidambaram, P., & O’Malley Watts, M. (2019). Key Questions About Medicaid Home and Community-Based Services Waiver Waiting Lists. Retrieved April 14, 2021, from https://www.kff.org/medicaid/issue-brief/key-questions-about-medicaid-home-and-community-based-services-waiver-waiting-lists/